Marrakech – Depression isn’t just sadness. It’s a neurochemical imbalance, a social disconnection, a body-level fatigue, and a cruel internal monologue all wrapped into one.
According to the World Health Organization, over 280 million people worldwide suffer from depression. So if you feel like you’ve been living under a raincloud, know this: you’re not alone, and yes — there is science-backed hope.
Let’s break down the healing journey, one research-based step at a time.
First, understand the biology: it’s not “all in your head” — except it kind of is.
Depression is linked to changes in the brain’s chemistry — specifically low levels of neurotransmitters like serotonin, dopamine, and norepinephrine.
It can also shrink the hippocampus, the part of your brain that regulates mood and memory.
A landmark study in The Journal of Neuroscience (Sheline et al., 1996) showed that individuals with chronic depression had smaller hippocampal volumes.
But the plot twist? Treatment — whether medication or therapy — can reverse that shrinkage.
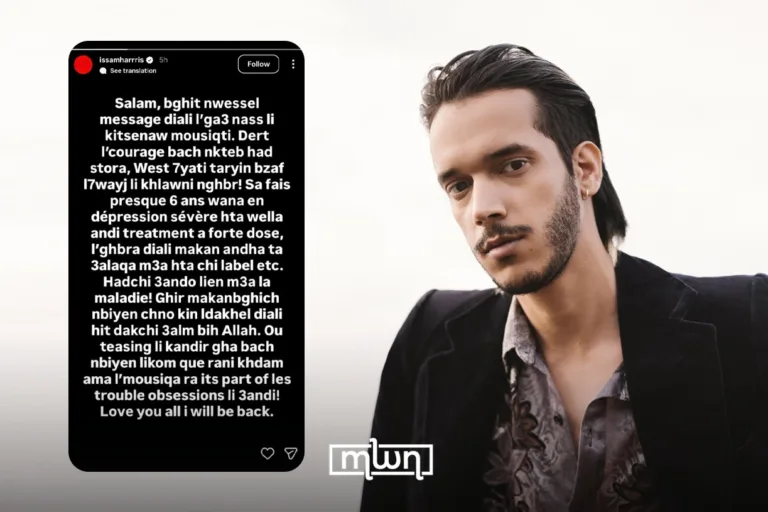
Sometimes, healing requires a little chemical help. Antidepressants like SSRIs (Selective Serotonin Reuptake Inhibitors) increase serotonin levels in the brain. According to the American Psychiatric Association, they work for about 60 to 70 percent of people.
But here’s the tea: they’re not happy pills. They’re scaffolding.
They support you while you climb — but you still have to climb. Think of it like getting a good bra — it won’t change your whole outfit, but the support can be transformative.
Therapy, especially Cognitive Behavioral Therapy (CBT), is the gold standard. It works by rewiring the thought patterns that drag you down.
A meta-analysis in Cognitive Therapy and Research (Cuijpers et al., 2013) found CBT to be as effective as antidepressants for many people — and even better at preventing relapse.
CBT teaches you to recognize your inner critic, label cognitive distortions (“I’m worthless” becomes “I’m having a bad day, not a bad life”), and reframe narratives.
In Carrie-speak: it’s like editing your inner monologue until it finally roots for you.
Exercise isn’t just for aesthetics or those weirdos who say they “like running.”
Moving your body actually increases brain-derived neurotrophic factor (BDNF), a protein that helps your brain grow and adapt.
A study in Psychosomatic Medicine (Blumenthal et al., 2007) showed that 30 minutes of aerobic exercise, three times a week, was as effective as Zoloft for treating major depression.
Translation: that walk you’re dreading? It’s literally medicine.
Sleep, sunlight, and diet form a boring but crucial trio. Poor sleep is both a symptom and a cause of depression.
Creating a wind-down routine and ditching doom-scrolling can help your brain get the REM it desperately needs.
Vitamin D deficiency is linked to mood disorders, and even 15 minutes a day in the sun can make a difference.
The gut-brain axis is real — omega-3 fatty acids, leafy greens, and probiotics can influence serotonin production.
Harvard Health reports that people who follow a Mediterranean diet have a 33 percent lower risk of depression.
Depression lies. It tells you no one cares. But science begs to differ.
According to a 2020 study in The Lancet Psychiatry, social support is one of the most protective factors against depression relapse.
Even texting a friend “thinking of you” counts. Vulnerability is terrifying — but it’s how the light gets in.
Modern science is also bringing bold new options: ketamine, once an anesthetic, is now a fast-acting antidepressant; psilocybin (magic mushrooms) may help “reset” the brain in clinical settings; and Transcranial Magnetic Stimulation (TMS) is a non-invasive way to stimulate mood-regulating brain areas.
Johns Hopkins and Yale are exploring these treatments with promising results—but these are not DIY options. Always go the clinical route.
In conclusion, healing isn’t linear, but it is possible.
Depression may be a sneaky liar, but science — and your own resilience — are louder.
Healing takes time, support, and often a mix of treatments.
You wouldn’t shame someone for taking insulin for diabetes — so why shame yourself for needing help for your mind?
If I’ve learned anything from science and my own moody mornings, it’s this: the brain, like the heart, wants to heal. It just needs a little help and a whole lot of love.
So whether it’s therapy, a morning walk, an SSRI, or a heartfelt chat with someone who truly sees you — keep reaching. The light is there.